Switching jobs? Your employer-sponsored health insurance could vanish unless you act fast! Discover IRDAI’s little-known portability rules to retain your group health cover, safeguard waiting-period credits, and avoid costly medical gaps. With India’s attrition at 20% and healthcare costs soaring 15% yearly, missing the 45–60-day window could mean fresh waiting periods for pre-existing conditions.
Switching jobs in India’s dynamic workforce is a thrilling leap toward new opportunities, career growth, and better prospects. Yet, amidst the excitement of a fresh start, a critical detail often slips through the cracks: your employer-sponsored health insurance could vanish the moment you resign. What if you could retain those hard-earned benefits, like waiting-period credits for pre-existing conditions, even after leaving your company? The good news is, you can—but only if you act swiftly.
This blog unravels the secrets of health insurance portability in India, guided by the Insurance Regulatory and Development Authority of India (IRDAI) 2025 guidelines. With health insurance penetration at just 37% of India’s population and medical costs soaring, retaining your corporate health cover is a financial lifeline. Read on to discover urgent steps, real-world cases, and expert tips to ensure your health benefits follow you seamlessly to your next career milestone.
The Hidden Risk of Losing Your Health Cover
When you resign, your group health insurance—a perk enjoyed by millions of salaried professionals in India—typically lapses. According to IRDAI’s 2024-25 Annual Report, approximately 514 million Indians (37% of the population) have some form of health insurance, with employer-sponsored plans covering a significant chunk. Yet, few employees realize they can port their group health cover into an individual plan, preserving benefits like waiting-period credits and no-claim bonuses.
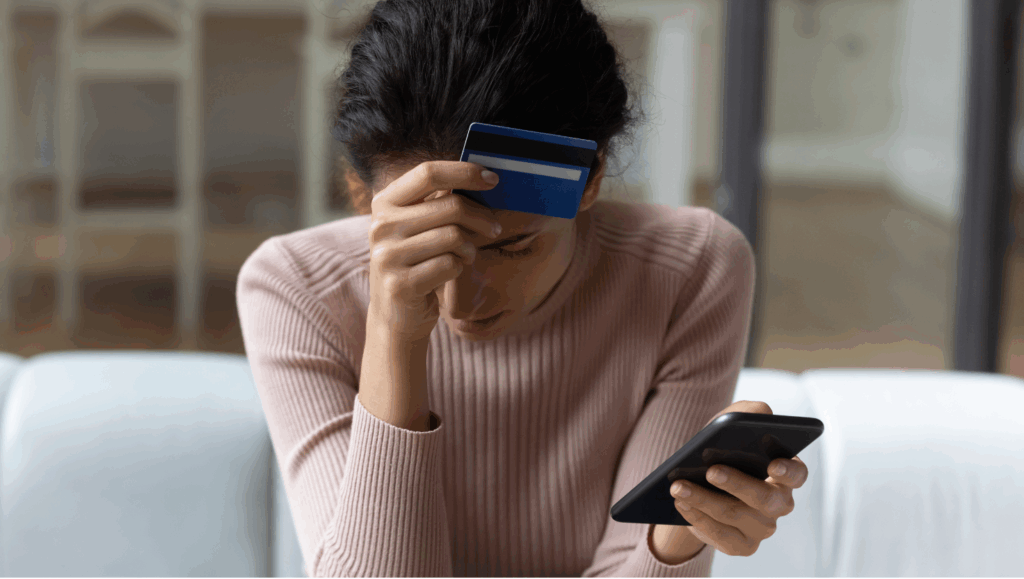
The stakes are high. India’s workforce is increasingly mobile, with attrition rates rising from 15.8% in 2020 to 19.7% in 2021, and stabilizing near 20% in 2024, driven by career shifts and better remuneration. As professionals chase new roles, a coverage gap can leave them vulnerable to spiralling medical costs, especially if pre-existing conditions like diabetes or hypertension are involved. With healthcare inflation climbing at 15% annually, a single hospital stay could wipe out savings.
Why does this matter? Imagine facing a medical emergency just after switching jobs, only to discover your new policy imposes a fresh waiting period for a condition you thought was covered. This blog reveals how to avoid such pitfalls by acting fast and leveraging IRDAI’s portability provisions.
What Is Health Insurance Portability?
Introduced in 2011, health insurance portability is a game-changer for Indian policyholders. Governed by the IRDAI (Health Insurance) Regulations, 2016, portability allows you to transfer your group health insurance to an individual or family floater plan without losing accrued benefits. Here’s what you can retain:
- Waiting-Period Credits: Time served under your group policy for pre-existing conditions carries over.
- No-Claim Bonus (NCB): Cumulative bonuses for claim-free years transfer to your new plan.
- Continuity of Coverage: Avoid fresh underwriting for conditions already covered.
In 2024, IRDAI reduced the waiting period for pre-existing diseases (PEDs) from four years to three years, making portability even more critical for those with chronic conditions like heart disease or renal issues. Over 100,000 policyholders utilized portability in recent years, reflecting growing awareness, yet millions remain unaware of this right.
Today’s Gold and Silver Prices in Bangalore, Hyderabad, Mumbai, Delhi: Guide for Buyers
February 18 Gold Silver Crash: How Rs 8000 Silver Fall Impacts Wedding Jewellers
The Evolution of Ola: From Startup to Prominent Brand
Central Bank of India Fixed Deposits: Maximize Wealth with 7.60% Interest Rates
Key IRDAI Portability Rules
To ensure a smooth transition, IRDAI mandates strict guidelines:
- Application Window: Submit your portability request 45–60 days before your group policy’s renewal date.
- No Extra Fees: Porting incurs no additional charges, though premiums may adjust based on age, sum insured, or underwriting.
- Continuity of Benefits: The new insurer must honour waiting-period credits and NCB from your group policy.
- Underwriting Discretion: The new insurer may review your medical history and claim record, potentially requiring health check-ups.
- Moratorium Period: After 60 months of continuous coverage, claims cannot be denied for non-disclosure (except fraud), preserving your policy’s value.
Miss these rules, and you risk starting from scratch with a new policy—potentially facing years of waiting periods for critical treatments.
Why Speed Is Non-Negotiable
The phrase “act fast” isn’t just a catchy tagline—it’s a necessity. Group health policies typically renew annually, and the 45–60-day window before renewal is your only chance to port without losing benefits. Delaying beyond this period means your application may be treated as a new policy, subjecting you to fresh waiting periods and underwriting scrutiny.
Consider Ritu, a 34-year-old marketing executive from Mumbai. Frustrated by claim delays in her employer’s group policy, she decided to port to an individual plan. But she applied just two weeks before renewal, missing the IRDAI-mandated window. Her new insurer treated her request as a fresh application, imposing a three-year waiting period for her chronic asthma treatment. This left Ritu facing ₹75,000 in out-of-pocket expenses for emergency care—a costly lesson in timing.
On the flip side, proactive planning can save the day. Priya, an HR manager in Delhi, initiated portability 75 days before her group policy’s renewal. She seamlessly converted her cover into a family floater plan, retaining credits for her husband’s diabetes treatment and saving ₹50,000 in premiums. The moral? Start early to secure your health shield.
Step-by-Step Guide to Retaining Your Health Cover
Navigating health insurance portability may seem daunting, but with the right steps, it’s straightforward. Follow this actionable guide to ensure a seamless transition:
1. Review Your Group Policy Immediately
Check your policy documents for the renewal date, sum insured, and waiting-period credits for pre-existing conditions. Request a portability certificate from your employer’s HR team, detailing your coverage history and claims. This ensures transparency when approaching the new insurer.
2. Notify HR and Insurer Simultaneously
Submit a written portability request to your current insurer at least 45 days before renewal, copying your HR department. Insurers must share your policy and claim history via IRDAI’s Insurance Information Bureau (IIB) portal within 72 hours. This centralized data-sharing ensures the new insurer has all necessary details.
3. Choose Your New Policy Wisely
Select an individual or family floater plan that matches or enhances your group policy’s benefits. Compare plans for cashless hospital networks, AYUSH coverage, and add-ons like critical illness riders. IRDAI’s 2024 guidelines removed sub-limits on AYUSH treatments, so explore plans covering Ayurveda, Yoga, or Homeopathy.
4. Confirm Acceptance and Premiums
The new insurer will review your application, claim history, and medical records within 15 days. They may request health check-ups, especially if you’re over 45 or have pre-existing conditions. Upon acceptance, verify the adjusted premium and ensure waiting-period credits transfer.
5. Bridge Coverage Gaps
If there’s a delay in finalizing portability, consider a short-term health insurance policy to cover interim medical needs. IRDAI allows a 30-day grace period for premium payments during porting, ensuring no lapse in coverage.
6. Maintain Documentation
Keep copies of all correspondence, portability certificates, and policy documents until your new plan is active. This protects you in case of disputes or delays.
Real-World Cases: Triumphs and Traps
The Near-Miss: A Costly Oversight
Amit, a 40-year-old IT professional in Bangalore, resigned to join a startup. Busy with his transition, he applied for portability just 12 days before his group policy’s renewal. His new insurer treated the request as a fresh application, imposing a two-year waiting period for his cataract surgery—despite Amit having served one year under his group plan. Forced to pay ₹1.2 lakh out-of-pocket for surgery, Amit’s emergency fund took a hit.
The Proactive Planner: A Success Story
Contrast this with Neha, a 38-year-old finance manager in Chennai. She notified her insurer 60 days before renewal, providing all required documents. Her group policy’s three-year waiting period for hypertension was fully credited, and she ported to a plan with a 15,000-hospital cashless network. When Neha needed emergency treatment, her new policy covered ₹80,000 in costs without delays.
These cases highlight a universal truth: timing is everything. Acting within the IRDAI window ensures your benefits remain intact, while delays can lead to financial strain.
The Bigger Picture: Why Portability Matters
India’s health insurance landscape is evolving rapidly. IRDAI’s 2024-25 guidelines have made policies more inclusive, with key changes:
- No Age Limits: Insurers must offer plans to all age groups, including senior citizens above 65.
- Reduced Waiting Periods: PED coverage now kicks in after three years, down from four.
- Non-Discrimination: Insurers cannot deny coverage for severe conditions like cancer or AIDS, subject to underwriting.
- Cashless Claims: Insurers must process cashless claims within one hour and settle within three hours post-discharge.
Despite these advancements, health insurance penetration remains low at 4.2% of GDP, with many unaware of portability options. As medical inflation outpaces general inflation, retaining your group cover’s benefits is a financial safety net. For instance, a single hospitalization for a critical illness can cost ₹1–5 lakh, making portability a smart move for professionals with chronic conditions or elderly dependents.
Common Pitfalls to Avoid
Porting isn’t fool proof. Here are mistakes to steer clear of:
- Missing the Deadline: Applying less than 45 days before renewal risks rejection or new waiting periods.
- Incomplete Documentation: Failing to provide claim history or medical records can delay or derail your application.
- Ignoring Policy Fine Print: Not all plans are portable (e.g., top-up plans can’t port to critical illness plans).
- Overlooking Underwriting: The new insurer may reject high-risk applicants or adjust premiums based on medical history.
To avoid these, consult a trusted insurance advisor or use different platforms to compare plans and streamline the process.
The Bottom Line: Secure Your Health Shield Now
Switching jobs is a bold step toward a brighter future, but don’t let it jeopardize your health insurance benefits. With India’s attrition rate hovering near 20% and medical costs rising relentlessly, portability is your shield against financial vulnerability. By acting within the 45–60-day window, you can:
- Safeguard Waiting-Period Credits: Ensure pre-existing conditions remain covered without delays.
- Maintain Continuity: Avoid gaps that expose you to out-of-pocket expenses.
- Preserve Bonuses: Retain no-claim bonuses for cost-effective premiums.
Don’t gamble with your health. Contact your HR team today, obtain your policy details, and notify your insurer to initiate portability. In a competitive job market, securing your health insurance portability ensures your health shield moves with you—seamlessly, affordably, and without skipping a beat.
Act now. Your next career milestone deserves the safety of uninterrupted health coverage.
With over 15 years of experience in Banking, investment banking, personal finance, or financial planning, Dkush has a knack for breaking down complex financial concepts into actionable, easy-to-understand advice. A MBA finance and a lifelong learner, Dkush is committed to helping readers achieve financial independence through smart budgeting, investing, and wealth-building strategies, Follow Dailyfinancial.in for practical tips and a roadmap to financial success!